A decades-long framework of American public health, credited with shielding generations of children from devastating illnesses, has been officially upended in favor of a new national experiment in parental choice and vaccine skepticism. The administration’s sudden and sweeping overhaul of the U.S. childhood immunization schedule represents one of the most significant public health pivots in modern history, directly translating years of controversial rhetoric into national policy. This monumental shift is now poised to test long-standing theories against the stark reality of infectious disease.
From Campaign Rhetoric to National Mandate: A High-Stakes Public Health Experiment Begins
In a decisive break from precedent, the administration has fundamentally altered the nation’s recommended childhood immunization schedule, reducing the number of diseases for which vaccination is universally advised from 17 to 11. This revision was implemented without the customary evaluation and vote from the independent panel of experts that has guided the Centers for Disease Control and Prevention (CDC) for decades. This departure from the established scientific review process signals a new era where policy is driven by administrative directive rather than consensus-based evidence.
This policy shift is widely seen as the direct implementation of Robert F. Kennedy Jr.’s long-professed skepticism toward the established vaccine schedule. What were once arguments made on the campaign trail and in public forums have now become the official stance of the federal government, setting up a direct confrontation with the overwhelming consensus of the global medical and scientific communities. The new mandate effectively launches a nationwide test of these theories, with the health of millions of children hanging in the balance.
The immediate reaction from pediatric and public health experts has been one of universal alarm. They predict that downgrading proven vaccines for diseases like influenza, meningitis, hepatitis A, and rotavirus will inevitably lead to lower vaccination rates, weaken community immunity, and trigger a resurgence of preventable illnesses. The following examination details the specific immunizations being reclassified and explores the profound risks associated with dismantling the very programs credited with conquering these diseases.
Dismantling the Shield: A Closer Look at the Downgraded Immunizations
Rescinding a Public Health Triumph: The Calculated Risk of Reclassifying the Hepatitis A Vaccine
The universal Hepatitis A vaccine program stands as a landmark public health achievement. Since its nationwide recommendation for children in 2006, the vaccine has been extraordinarily effective, contributing to a staggering 95% reduction in cases of the viral liver infection between 1996 and 2011, according to CDC data. With current uptake for the two-dose series reaching 80% among young children, the program has successfully contained a disease that once posed a significant threat.
However, the decision to rescind the universal recommendation reintroduces a serious and preventable risk. Hepatitis A spreads easily through contaminated food and water, making it a persistent threat that is difficult to control without widespread immunity. Public health officials argue that removing the vaccine from the standard schedule for most children dismantles a critical firewall against outbreaks, which can fluctuate wildly; nearly 19,000 cases were reported as recently as 2019, underscoring the virus’s potential to reemerge.
The rationale for downgrading a vaccine with such a proven track record remains a point of intense debate. Medical experts question the logic of moving a highly successful and widely accepted immunization to a risk-based model, arguing that it needlessly exposes the broader population. By shifting the vaccine from a universal standard to a selective recommendation, the policy gambles with a public health victory that was decades in the making.
From Universal Safeguard to Parental Choice: Why the Annual Flu Shot Is No Longer a Standard Recommendation
Influenza is far from a minor illness for children, a fact underscored by the severe 2024-2025 season that resulted in 289 pediatric deaths, the vast majority occurring in unvaccinated children. With projections indicating the current 2025-2026 season will be similarly severe, the annual flu shot has been a cornerstone of pediatric preventative care, aimed at mitigating the virus’s deadly impact on the young and vulnerable.
The administration’s new policy eliminates the universal recommendation for an annual flu shot, reclassifying it as a matter for “shared clinical decision-making.” This places the burden of initiation squarely on parents, who must now navigate complex risk assessments with their providers rather than receiving a clear public health directive. This shift is expected to accelerate the decade-long decline in pediatric flu vaccination rates, which have already fallen to just 42.5%, far below the 70% national health goal.
This change arrives at a precarious moment. By weakening the primary tool for building community-wide protection against influenza, the policy significantly increases the risk of widespread outbreaks. As flu activity intensifies across the country, public health experts warn that lower vaccination coverage will translate directly into higher rates of severe illness, pediatric hospitalizations, and preventable deaths, straining an already taxed healthcare system.
Confronting a Resurging Threat: The Unforeseen Consequences of Downgrading the Meningitis Shot
The assumption that meningococcal disease is too rare to necessitate universal vaccination is being directly challenged by emerging data. The U.S. saw the highest number of reported cases in over a decade in 2024, signaling that this dangerous bacterial infection may be on the rise. Known for causing meningitis, an inflammation of the brain and spinal cord, the disease can be swift and deadly, making prevention a critical priority.
Meningitis is particularly notorious for causing devastating outbreaks in close-contact environments such as college dormitories and military barracks, where the disease can spread rapidly through saliva. The high vaccination rate for the MenACWY vaccine—with over 90% of teenagers receiving at least one dose—has been the key defense against such scenarios. This high level of coverage creates a powerful shield of herd immunity that protects entire communities.
The decision to downgrade this vaccine to a “shared clinical decision-making” model fundamentally misreads the dynamics of infectious disease prevention. The policy’s logic is circular: the vaccine appears non-essential precisely because its high uptake has made the disease rare. By dismantling the universal recommendation, the administration risks a rapid decline in coverage, creating the exact conditions needed for deadly outbreaks to return among a new generation of unprotected teens.
Turning Back the Clock on Infant Health: The Peril of Removing the Rotavirus Vaccine from the Standard Schedule
Before the introduction of the rotavirus vaccine, the virus was a leading cause of severe illness in American infants. Each year, it was responsible for 55,000 to 70,000 hospitalizations and dozens of deaths due to extreme dehydration from vomiting and diarrhea. Today, the vaccine prevents an estimated 45,000 of those hospitalizations annually and protects about 90% of vaccinated children from severe disease, marking a profound victory for infant health.
Withdrawing the routine recommendation for this vaccine for infants—the population most vulnerable to its effects—is a move that pediatric specialists warn could swiftly overwhelm hospitals. Rotavirus is highly contagious and spreads with ease through settings like daycare centers. Without the protective barrier of routine vaccination, experts anticipate a swift return to an era where pediatric wards are filled with infants suffering from life-threatening dehydration.
The future trajectory of rotavirus is now uncertain. By deliberately setting aside one of the most effective tools for its containment, the new policy risks transforming a well-managed disease back into a rampant public health crisis. The reclassification of this vaccine essentially initiates an uncontrolled experiment to see if a society can maintain control over a highly infectious pathogen after abandoning its most effective defense.
Navigating the New Normal: Expert Warnings and Practical Guidance for Parents
The consensus from the medical and public health communities is clear and unequivocal: the administration’s new vaccine policy is not supported by scientific evidence and is expected to result in a significant increase in preventable disease, hospitalizations, and child deaths. Experts emphasize that the downgraded vaccines are safe, effective, and crucial for both individual and community health. They warn that this policy shift will create confusion, amplify vaccine hesitancy, and ultimately reverse decades of progress.
In this new landscape of conflicting public health messages, parents face the challenge of making informed decisions for their children. The most critical strategy is to maintain a strong relationship with a trusted pediatrician. Parents are encouraged to proactively schedule consultations to discuss the established science behind each downgraded vaccine, understand the specific risks posed by these diseases in their community, and develop an immunization plan based on medical guidance rather than political ideology.
Healthcare providers, in turn, are being called upon to redouble their efforts in family counseling. Best practices include clearly and patiently communicating the robust evidence supporting the safety and efficacy of the Hepatitis A, influenza, meningitis, and rotavirus vaccines. By reaffirming the established science and contextualizing the risks of non-vaccination, pediatricians can serve as a vital source of clarity and stability for families navigating this unprecedented and confusing new normal.
The Unfolding Experiment: Measuring the True Cost of a New Vaccine Philosophy
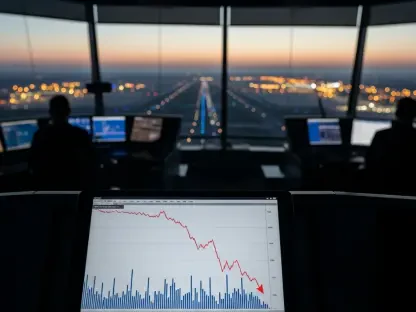
At its core, the new national immunization policy represents a real-time test of a political ideology, with the health and safety of children serving as the primary outcome measure. The administration is effectively wagering that its theories on vaccine safety and necessity are more accurate than the collected evidence and experience of the global public health community. The results of this wager will not be academic; they will be measured in hospital admission rates and disease incidence reports.
The long-term implications of this experiment extend far beyond individual infections. Waning vaccination rates threaten to erode the herd immunity that protects the entire population, especially the most vulnerable, such as infants too young to be vaccinated and individuals with compromised immune systems. This could pave the way for the re-emergence of diseases that have been so effectively controlled for generations that many Americans no longer recognize them as serious threats.
This situation demands unprecedented vigilance. As this high-stakes public health experiment unfolds, the responsibility falls to public health officials, healthcare providers, and parents to closely monitor disease surveillance data. These statistics will provide the first, undeniable indicators of the real-world impact of this new vaccine philosophy. The cost of this policy will ultimately be tallied not in dollars, but in the preventable illnesses and tragic outcomes that may follow.