Amidst rapid technological advancements that promise unparalleled efficiency, the frontline staff administering the nation’s Medicaid programs remain mired in outdated processes that hinder their ability to deliver timely and critical healthcare access to millions. This research summary delves into the potential of Artificial Intelligence (AI) to transform this landscape, not by replacing human expertise, but by augmenting it. The central argument presented is that the successful integration of AI into public benefits administration is contingent upon a human-centered design philosophy that prioritizes the daily operational needs of frontline eligibility workers. By focusing on the critical, yet often overlooked, role of the staff who manage these complex systems, it becomes clear that empowering these individuals is the most effective path to modernizing government services and improving the system for everyone involved, from state agencies to the residents they serve.
A Human-Centered Approach to AI in Public Benefits
The conversation surrounding AI in government services frequently gravitates toward high-level goals of cost savings and administrative efficiency. However, a more effective and sustainable approach begins with a granular understanding of the day-to-day work of those on the front lines. This analysis examines how a human-centered design, which places the eligibility worker at the core of technological development, can unlock the true potential of AI. Instead of implementing technology that simply automates processes from a top-down perspective, this approach advocates for tools that directly address the specific frustrations and bottlenecks that staff encounter. The successful adoption of AI, therefore, depends less on the sophistication of the algorithm and more on its ability to seamlessly integrate into and improve the existing human workflow.
Modernizing government services presents a formidable challenge, often stymied by legacy systems and entrenched bureaucratic processes. A common misstep is to focus technological investment on large-scale system overhauls that fail to consider the human element of service delivery. The core premise of this research is that empowering eligibility workers with targeted, intelligent tools creates a ripple effect of positive change. When workers are freed from tedious administrative tasks and equipped with better information, they can dedicate more time and cognitive energy to the complex, nuanced aspects of their jobs, such as verifying complex household situations and providing empathetic support to clients. This shift in focus not only improves efficiency and accuracy but also enhances the quality of interaction between the government and the public, fostering a more humane and responsive social safety net.
The Critical, Overlooked Role of the Eligibility Worker
Eligibility workers function as the essential human interface for state Medicaid programs. They are the conduits through which residents access vital healthcare, navigating a labyrinth of complex regulations and often disjointed technological systems on behalf of applicants. Their responsibilities are vast, ranging from processing initial applications and verifying documentation to answering a constant stream of questions and guiding families through the intricate and often stressful enrollment and redetermination processes. They are simultaneously case managers, policy interpreters, and client advocates, making their role indispensable to the proper functioning of the nation’s social safety net.
Despite their critical importance, these workers face significant and pervasive systemic obstacles that undermine their effectiveness and lead to negative outcomes for the entire system. This research is significant because it illuminates the direct link between worker challenges and public service failures. Overwhelming administrative burdens, fragmented and non-communicating technology, and constant policy changes contribute to high rates of burnout, create operational inefficiencies, and result in unacceptable delays in service delivery. Understanding and solving the deeply entrenched problems that eligibility workers encounter every day is therefore not merely an issue of internal process improvement; it is a crucial step toward enhancing the efficiency, accuracy, and accessibility of Medicaid for the millions of Americans who depend on it.
Research Methodology, Findings, and Implications
Methodology
The research presented here is grounded in a qualitative analysis of expert testimony and strategic recommendations from leading policy and data science professionals at a nonprofit organization dedicated to improving government services through technology. The methodology involved a careful synthesis of their collective insights, which were derived from extensive work with state agencies and frontline staff. This approach focused on identifying the primary challenges and operational pain points that consistently hinder the performance of eligibility workers across different jurisdictions. Subsequently, the analysis evaluated the feasibility and potential impact of their proposed AI-powered solutions, which are specifically targeted to address these identified problems in a practical and worker-centric manner.
Findings
The research identified three primary operational pain points that severely impede the effectiveness and efficiency of Medicaid eligibility workers. The first and most pervasive issue is the staggering burden of duplicative and manual data entry. Workers are frequently compelled to input the same client information repeatedly across multiple, non-communicating legacy systems. This redundant, clerical labor consumes a disproportionate amount of their time and energy, diverting their focus from the more analytical and human-centered aspects of their roles. This systemic flaw not only slows down application processing but also increases the likelihood of data entry errors, which can have serious consequences for applicants.
A second major finding is the profound difficulty workers experience when trying to navigate complex and siloed state data infrastructures. In order to get a complete and accurate view of a case, an eligibility worker must often act as a digital detective, piecing together information from various databases that store information inconsistently. For example, a single applicant’s name, address, or phone number might be recorded in several different formats across separate systems, forcing the worker to spend valuable time reconciling these discrepancies. This fragmentation of data makes it exceedingly difficult to form a unified client profile, leading to a cumbersome and error-prone verification process that can delay or jeopardize an individual’s access to care.
Finally, the research highlights the immense cognitive load placed upon eligibility workers due to chronic information overload. These professionals must maintain an expert-level understanding of a vast and constantly evolving body of complex Medicaid policies, program rules, and legal requirements. Concurrently, they must absorb and process a high volume of detailed, personal data for each client case they handle. A significant portion of their job involves translating dense, jargon-laden policy language into clear, understandable terms for applicants. This dual burden of managing institutional knowledge while processing client-specific information can be overwhelming, contributing to stress and creating communication barriers that hinder successful enrollment.
Implications
The findings point toward a clear and actionable path forward for state agencies, with specific, practical AI applications that can be deployed to solve each of the identified problems. To address the burden of manual data entry, the primary implication is the adoption of AI-enabled data extraction tools. This technology can automate the tedious work of reading and processing information from scanned documents and other unstructured sources, pre-populating forms and shifting the worker’s role from data entry to the more critical task of verification. This single change can dramatically improve both the speed and accuracy of the initial application stages.
Moreover, the challenge of siloed data implies a need for leveraging AI-powered entity resolution. This technique can automatically identify and link different records pertaining to the same individual across disparate systems, creating a single, unified client profile. Providing workers with a comprehensive and reliable view of a case eliminates the need for manual detective work and ensures that eligibility decisions are based on a complete set of information. In parallel, the issue of information overload suggests the deployment of generative AI. These models can be used to summarize complex policy documents into plain language, create more effective training materials, and generate clearer communications for applicants, directly improving comprehension for both staff and the public they serve.
Reflection and Future Directions
Reflection
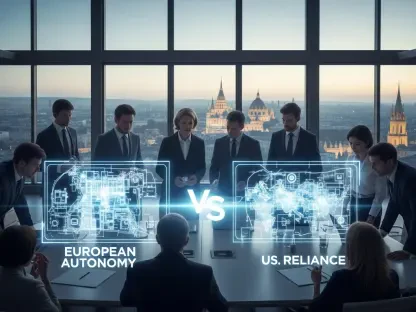
This analysis brings a common pitfall in government technology projects into sharp focus: an overwhelming tendency to concentrate on the needs of high-level stakeholders, such as agency leaders and vendors, while neglecting the practical, on-the-ground realities of frontline staff. A key challenge in implementing these promising AI solutions will be to overcome the powerful inertia of legacy systems and the procurement processes that perpetuate them. Fostering a culture of co-design, where eligibility workers are treated not as subjects of change but as essential partners in technological development, will be paramount to success. This research ultimately underscores a fundamental principle of effective modernization: technology must be designed to serve the user, not the other way around.
Future Directions
Looking ahead, future research must prioritize the implementation of pilot programs designed to quantitatively measure the impact of these worker-centric AI tools. Rigorous evaluation is needed to assess their effects on key performance metrics, including application processing times, error rates in eligibility determinations, worker satisfaction and retention, and, most importantly, client outcomes. Tracking these indicators will provide the concrete evidence that state leaders need to justify broader investment in these human-centered technologies.
Furthermore, additional exploration is urgently needed to develop robust ethical frameworks for the deployment of AI in social safety net programs. As these powerful tools become more integrated into eligibility systems, it is essential to establish clear guidelines and oversight mechanisms to ensure fairness, transparency, and accountability. Future work should investigate methods for auditing AI-driven processes for bias, establishing clear appeals processes for citizens affected by automated decisions, and ensuring that the use of AI enhances, rather than erodes, the public’s trust in government services.
Conclusion Shifting from Administrative Efficiency to Human-Centered Empowerment
In summary, the potential for AI to transform Medicaid administration was found to be immense, but its success was entirely dependent on a strategic shift in focus. The research concluded that designing technology to directly empower eligibility workers, rather than simply pursuing abstract efficiencies, yielded the most promising results. By developing and deploying tools that were precisely targeted to alleviate daily frustrations and automate the most tedious and error-prone tasks, state agencies could achieve the dual goals of streamlining complex administrative processes and significantly improving the experience of applicants and enrollees. Ultimately, building a more humane and effective Medicaid system began with empowering the people who served on its front lines.